Osteoporosis
and Gluten
By James Braly, M.D. and Ron Hoggan, M.A. Dangerous Grains
More on Osteoporosis
I was diagnosed about thirteen years ago with celiac. I weighed 112 pounds, and I am six feet one inch tall. I was still walking/ working, but barely. I had stress fractures in my feet. My vision had
deteriorated to the point where I was getting a new prescription about every six months. I was having nosebleeds every day along with headaches, abdominal cramps, leg cramps, muscle twitching,
tingling in my fingers and toes, bone pain, etc. About three days after going gluten free, I felt better. I had to get new prescriptions on my glasses about every
six
months due to vision improvement. My hair grew back. I gained about 60 pounds over three years.
Jim B.
 If you have weak, porous bones, you might want to eliminate gluten from your diet even if you do not mount an immune response to this food. A significant portion of our society is plagued by this
silent disability. The first painful hint of a problem is often a broken bone. There are several ways that gluten can interfere with maintaining strong, healthy bones. In this chapter, we explain how
gluten can cause this crippling and painful malady.
If you have weak, porous bones, you might want to eliminate gluten from your diet even if you do not mount an immune response to this food. A significant portion of our society is plagued by this
silent disability. The first painful hint of a problem is often a broken bone. There are several ways that gluten can interfere with maintaining strong, healthy bones. In this chapter, we explain how
gluten can cause this crippling and painful malady.
According to the National Osteoporosis Foundation, osteoporosis is a major public health threat for more than 28 million Americans, 80 percent of whom are women. In the United States today, 8 million women and 2 million men already have osteoporosis, and 18 million more have low bone density, placing them at increased risk for osteoporosis; hip, back, and wrist fractures; and premature death.
Approximately 250,000 Americans die annually from the complications associated with hip fractures. Co-author James Braly's father was one such osteoporotic hip fracture victim.
Cases of bone degeneration are increasing at an epidemic rate. Much of it is due to our aging population, of course, with women now living well beyond eighty and men following closely behind. But that is only part of the explanation. Current dietary recommendations are shortsighted and out of date, reflecting a simplistic view of the many factors that contribute to building and maintaining strong, healthy bones.
The source of much of this poor advice is the infamous USDA food guide pyramid. Its proponents have failed to keep pace with current research. Despite exploding numbers of cases of osteoporosis and the well documented, negative impact of gluten consumption on bone density, daily consumption of six to eleven servings of cereal is still recommended Such recommendations are akin to urging a drowning man to drink more water. These recommendations are a clear denial of much of what we now know about bones, how they grow, and what makes them strong.
Gluten can also cause osteoporosis in the non-gluten sensitive
Phytate is the storage form of most phosphorus found in plants. It has a strong
attraction to a variety of minerals including calcium, magnesium, iron and zinc.
Even for people who do not suffer from gluten sensitivity~ phytates are cause for
concern. They are found in large quantities in the outer layer of cereal grains. During digestion, especially in the stomach, phytates will combine with calcium
and other minerals. The bonds that form in these chemical combinations are
resistant to the human digestive process, so important minerals will be wasted
when phytates are consumed. Therefore, by eating whole grains we decrease the
availability of those dietary minerals that help us grow and maintain strong,
healthy bones.
Vitamin K chlorophyll liquid or capsules) is deficient in the diets of many women, many celiacs, and most people suffering from osteoporosis. At one time, vitamin K, an essential vitamin derived from food and the action of intestinal bacteria, was thought to be involved solely with the clotting of blood. As it turns out, vitamin K is needed in other key processes, including the production of osteocalcin by osteoblasts. Osteocalcin is a bone protein important in bone metabolism and bone formation. When excessive levels are found in the blood, it is associated with bone disorders such as Paget's disease and postmenopausal osteoporosis.
The January 1999 issue of the American Journal of Clinical Nutrition reported on more than seventy-two thousand women who were divided on the basis of their consumption of vitamin K. Those who consumed the most vitamin K were only 70 percent as likely to have broken a hip as women in the group that took in the least amount of this important vitamin. More impressive was the observation of lettuce consumption. Women who ate vitamin K-rich lettuce at least once a day were 45 percent less likely to have a hip fracture than those who ate the same food once a week or less. Consuming less than 109 micrograms of vitamin K resulted in bone thinning, but more than 109 micrograms did not add any more protection against hip fracture.
For women ages fifteen and older, federal guidelines recommend consuming 180 micrograms of vitamin K each day, probably an excessive amount. On the other hand, the RDA for vitamin K is 65 micrograms for women and 80 micrograms for men, which is probably too low.
The research findings clearly demonstrate that other nutrients besides calcium are
important for maintaining healthy bones. Instead of the current narrow focus on calcium, women ought to be sure to eat a well-balanced diet containing enough
protein and vitamin K. In addition to broccoli, lettuce, and other leafy vegetables, foods rich in vitamin K include pork, liver, and vegetable oils.
Vitamin A deficiency, another problem that often arises from gluten consumption,
can cause stunted growth in children and can also impact on adult bones. Because this vitamin coordinates both bone-building and bone-destroying cells,
a deficiency may cause a wide range of bone abnormalities. To ensure sufficient vitamin A in your diet, eat foods such as fish, flax, and liver, which are rich in this important vitamin.
 Bones are very much alive
Bones are very much alive
Bones are living tissue. Calcium, magnesium, zinc, and other minerals are deposited and removed on an ongoing basis. Connective tissues within bones and
supporting the bones are renewed regularly. This work is conducted by cells that are bone builders (osteoblasts) and cells that are bone
destroyers (osteoclasts). Our bones are made up of about 25 percent water, 25
percent protein, and the rest are mineral salts, mostly calcium. Collagen is the
connective tissue that provides the flexible framework on which these brittle
mineral salts crystallize.
In healthy bones, this combination results in strong,
somewhat flexible bones. The minerals provide rigidity, and the collagen
provides flexibility while reinforcing the minerals, much like the principles that
give reinforced concrete its strength.
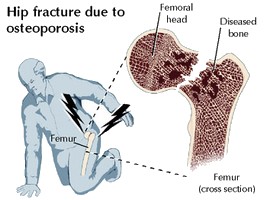
What is osteoporosis?
When our bones are broken by mild impact or by normal, day-to-day stresses,
they are not healthy. Weak bones usually have more and larger spaces between
the mineral crystals that weaken bones by making them porous. By now, it will
be no surprise for you to learn that gluten can cause this terrible, debilitating
condition. Contrary to the current, unfortunate dietary fad, dairy products may
also be contributing to many cases of osteoporosis. Adult-diagnosed celiac invariably suffer some degree of demineralization of their
bones. The extent of this damage can be quite dramatic.
What causes osteoporosis in celiac patients?
For a long time, it was assumed that widespread osteoporosis among celiacs was
the result of malabsorption. While it makes sense that we would be unable to
absorb enough calcium, resulting in a deficiency, when researchers looked more
closely at this issue they found that the evidence doesn't support such a
simplistic view. It seems that gluten has a greater impact on calcium metabolism
than on actual absorption because it increases how much calcium we waste after
it is absorbed. A gluten-free diet often results in dramatic improvements to the mineral content of celiac
patients' bones, but this is largely due to increased retention of calcium.
A related paradox of osteoporosis and celiac disease is that calcium supplementation does not help to remineralize celiac patients' bones as much as magnesium supplementation. There is comparatively much less magnesium in our bones, so this information provides an important clue to the fascinating puzzle of the impact that gluten can have on bone density.
Not only is magnesium important to the activation of bone-building osteoblasts that deposit calcium and add collagen to our bones but is also a factor that aids in repairing the parathyroid gland. This is a gland that produces the hormones (PTH) that regulate most of the body's calcium metabolism. These hormones signal the kidneys to recover calcium from the urine, to elevate blood levels of calcium, and to activate vitamin D (calcitrol), which signals the intestine to absorb calcium from the food we eat. Clearly, adequate dietary calcium is of little value if we are not getting enough magnesium for the parathyroid gland to function properly.
For these reasons, dairy products and calcium supplementation may actually have a negative impact on the density of our bones, exactly the opposite of what we were taught to expect. It also counters the simplistic advice to consume calcium supplements alone and/or dairy products that are often offered to many individuals with declining bone density. Magnesium, calcium, zinc, boron, and vitamins D and K, all reported to be deficient in many celiacs, are absorbed from the intestine by the same mechanism, called "active transport." Loading the digestive tract with calcium alone overwhelmingly invites this part of our absorptive capacity with a single mineral, albeit the most common one in the body. This approach is shortsighted and, quite frankly, harmful. It risks causing a deficiency of magnesium and other necessary minerals, which are less abundant and frequently deficient in our diets. Magnesium and phosphorous deficiencies caused by excessive calcium intake may pose a much greater risk of causing bone mineral loss. Further, the risk is largely independent of the traditional suspect in gluten-induced bone damage malabsorption. The key issue is the balance of relative quantities in which these minerals are available, either in our diets and/or the supplements we consume.
Great care should be taken in recommending calcium/supplementation, especially among those who already suffer from bone demineralization and among those at greatest risk of developing such problems. A typical, healthy intestine only absorbs a small portion of the calcium that is available from our food. At the same time, evidence suggests that excess calcium intake competes with magnesium absorption, further aggravating a poor magnesium status. Flooding our diet with more and more calcium is a dangerously simplistic approach to this complex problem.
Many hospital emergency rooms are now using large therapeutic doses of intravenous magnesium as one of the first-line therapies for cardiac patients. Such magnesium treatments have been shown to reduce the extent of damage to the heart muscles and tissues. More and more medical clinics and emergency rooms are also beginning to use IV magnesium as a first-line therapy to abort migraine headaches and asthma attacks. The effectiveness of these therapies also suggests a common condition of chronic magnesium deficiency. We view this common deficiency as a predictable result of our culture's obsession with magnesium-depleting consumption of massive quantities of dairy products and cereal grains.
The parathyroid gland
Recall that, in untreated celiac disease, the parathyroid gland releases an excess of parathyroid hormone, the
single most important hormone for regulating calcium metabolism. This is associated with abnormally high bone
turnover and bone loss. We now have evidence that, at least in some cases of celiac disease, endomysium
antibodies (the same ones that are sought in screening tests for celiac disease) will cross-react with parathyroid
tissues, resulting in damage to this important gland and compromising its ability to effectively regulate our
calcium metabolism. Thinning of the bone, increased bone fragility, and proneness to low-impact bone fractures are the consequences.
The tragic underdiagnosis of celiac disease and gluten sensitivity certainly suggests the need for more frequent screening for these conditions among those with reduced bone density. Such testing should be conducted as early as possible to allow early and extensive gains in mineral deposition, resulting in strong, healthy bones prior to declining production of sex hormones and growth hormones later in life.
Osteomalacia and gluten
Another bone-density ailment that can also be related to gluten consumption is osteomalacia. This is a condition
where the bones are very flexible and weak. There appears to be ample collagen, but calcium, phosphorus, and/or
other necessary minerals for bone hardness are lacking. The childhood equivalent of osteomalacid is rickets.
Both are often the result of deficiencies in vitamin D. Recall that it is the active form of vitamin D, calcitrol, that
signals the intestine to absorb more calcium and other minerals from our food.
In osteomalacia and its milder form, osteopenia, our bones bend and become deformed due to a deficiency of absorbed minerals, and this condition can often be halted and reversed by simple vitamin D supplementation. Unfortunately, bone deformations usually are not corrected. Those who get little exposure to unimpeded sunlight, perhaps due to their jobs, age, or medical condition, are at risk. Those who live in temperate zones of the world run a seasonal risk of developing this problem.
Impaired kidney function, where there is excessive calcium excretion, can also result in rickets, osteornalacia, and
osteopenia. There is clear evidence that gluten contributes to at least some cases of impaired kidney function.
In an abstract entitled "Vitamin D: Importance in the prevention of cancers, Type I diabetes, heart disease, and osteoporosis" published in the American Journal of Clinical Nutrition, Michael F. Holick is quoted saying that "Studies in both human and animal models add strength to the hypothesis that the unrecognized epidemic of vitamin D deficiency worldwide is a contributing factor of many chronic debilitating diseases."
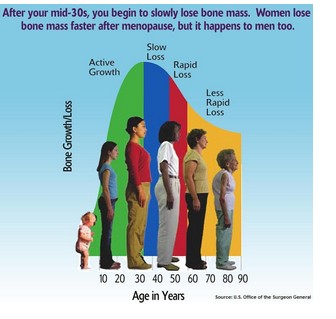
The impact of aging and sex hormones on bone health
All of the above factors in building and maintaining dense, healthy bones
become increasingly important as we approach middle age. The sex hormones
estrogen and testosterone stimulate the action of bone-building osteoblasts. As
women experience menopause and men approach their sixties, production of
these sex hormones is reduced. Bone building therefore slows and begins to be
outstripped by bone destruction. If we have built up strong bones in our early
years, if we continue with weight bearing exercise regularly, and if we are eating
and absorbing adequate quantities and an appropriate balance of all the
necessary minerals, our bones should continue to serve us throughout our old
age. If we are gluten sensitive or have celiac disease, even if religiously pursuing
a gluten-free diet, we may need to take aggressive action, supplementing
magnesium and ensuring adequate vitamin D intake or absorption. If you have a personal history of osteoporosis or osteopenia, periodic bone density tests should be done to assure that your gluten-free diet and
supplementation program are working optimally for you.
Back to the future
Gluten and dairy products are two of the most allergenic foods in our food
supply. As we have shown, calcium supplements as a primary or sole nutrient
intervention and consumption of gluten and dairy products can actually threaten
our absorption of other important minerals, compromise our bones and general
health, and cause the very disease they are purported to prevent.
As you have seen, there are many factors that affect bone health. Regular exercise, ample sunshine, a varied non-allergenic diet, and a variety of vitamins are needed, along with several important minerals and hormones. All of these factors must work in a balanced, harmonious manner to build and maintain strong bones. Any change in this balance can lead to sudden and measurable changes in a relatively short time. Substantial improvements in bone density occur within one year of diagnosing celiac disease and beginning a gluten-free diet. Excessive calcium supplementation, without a balance of other bone nutrients, may well contribute to the very problem that it is aimed at helping.
A gluten-free, dairy-free diet that includes a wide range of meats, organ meat, fish; poultry, vegetables, and fruits, with moderate quantities of non-gluten grains, is not only closer to the one we evolved to eat but also one that will give us strong, healthy bones. Given the importance of an optimally functioning parathyroid gland for bone health, the cross reaction between endomysium antibodies and the parathyrod gland also suggests that there may be autoimmune factors contributing to the bone damage caused by gluten.
|